Overview: HIPAA Compliance and Medical Billing in 2025
Table of Contents
ToggleMedical billing is a multi-stage process, starting from patient registration to claim resolution, often spanning several months.
HIPAA compliance is mandatory at every step of the billing process, particularly where electronic Protected Health Information (ePHI) is involved.
Compliance must cover the HIPAA Privacy Rule, Security Rule, and Breach Notification Rule.
Privacy Rule ensures proper use/disclosure of PHI and respects patients’ rights to access and amend their data.
Security Rule requires administrative, physical, and technical safeguards for handling ePHI.
The Breach Notification Rule mandates timely reporting of data breaches, and sometimes state laws may impose stricter timelines.
Inhouse billing (performed by internal staff) does not require Business Associate Agreements (BAAs), but must still follow HIPAA standards.
Outsourced billing (third-party providers) requires BAAs and strict controls since they are classified as Business Associates under HIPAA.
Medical debt is a growing issue—over $220 billion as of 2021—triggering new compliance measures through local/state regulations.
Organizations must comply not only with HIPAA, but also with local laws (e.g., billing caps based on income).
A comprehensive compliance strategy should include policies, secure technology, staff training, and proper documentation.
What Is the Relationship Between HIPAA Compliance and Medical Billing?
HIPAA compliance and medical billing are deeply interconnected due to the handling of sensitive patient information throughout the billing process.
Medical billing involves a series of complex administrative and clinical tasks, all of which require strict adherence to HIPAA rules, particularly the Privacy Rule, Security Rule, and Breach Notification Rule.
Compliance requirements vary depending on whether billing is handled inhouse or outsourced, and organizations must also consider state-specific regulations that may impose stricter privacy or reporting standards.
With the rising issue of medical debt, additional local measures may affect billing compliance. Ultimately, protecting electronic Protected Health Information (ePHI) is central to both accurate billing and HIPAA adherence.
What Does Medical Billing Involve?
Medical billing begins before any claim is submitted, starting at patient registration.
Steps include:
Collecting demographic and insurance information.
Conducting eligibility checks with health plans.
Determining copays, coinsurance, and deductibles.
Generating encounter forms and recording patient payments.
Coding clinical data into billable claims.
Submitting, tracking, correcting, and appealing claims over time.
Medical billing is not a one-time transaction—it’s a multi-stage process that can span several months, with many touchpoints involving ePHI.
How Does HIPAA Apply Throughout the Medical Billing Process?
HIPAA applies to every stage of medical billing, ensuring that individually identifiable health information is handled securely and ethically.
Privacy Rule Compliance
Applies to oral and written forms of Protected Health Information (PHI).
Key requirements:
General Principles of use and disclosure of PHI.
Adherence to the Minimum Necessary Standard.
Respect for patient rights to access and correct their health records.
Security Rule Compliance
Applies to electronic PHI (ePHI).
Covered entities and business associates must implement:
Administrative safeguards (e.g., risk analysis).
Physical safeguards (e.g., facility access controls).
Technical safeguards (e.g., encryption, access control).
Maintain Business Associate Agreements (BAAs) where necessary.
Follow HIPAA-compliant documentation and retention policies.
Breach Notification Rule
Requires procedures for detecting, reporting, and notifying individuals and authorities about data breaches.
Note: Some state laws may require quicker notifications than HIPAA mandates.
Organizations must comply with the stricter standard where state and federal rules conflict.
What’s the Difference Between Inhouse and Outsourced Medical Billing in Terms of HIPAA?
Inhouse Billing
Conducted by staff employed by the healthcare organization (covered entity).
No need for a Business Associate Agreement since billing staff are part of the workforce.
Allows direct communication between billers and physicians.
Still requires:
Minimum Necessary Standard enforcement.
Use of secure internal communication tools.

Latest Blog
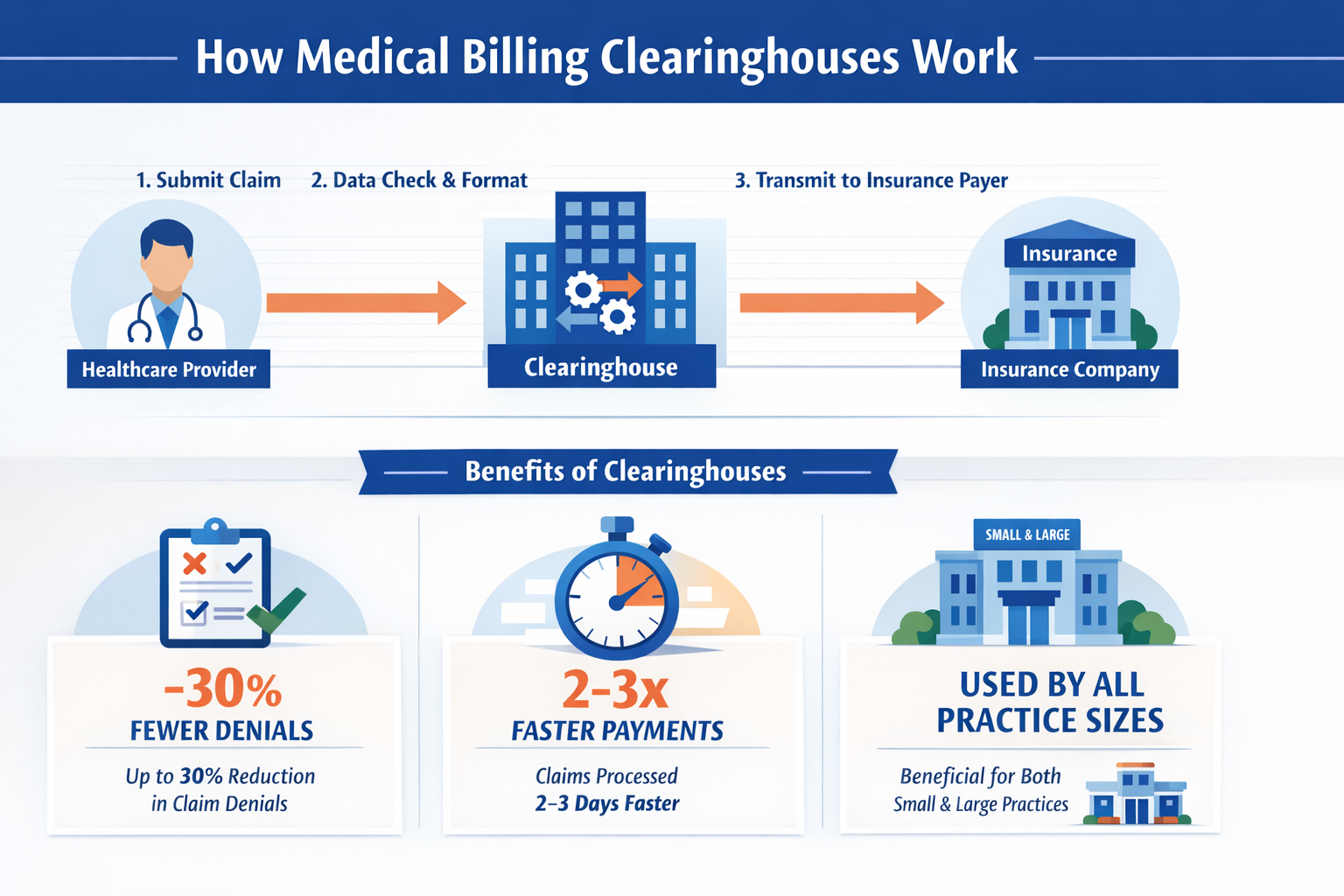
Outsourced Billing
Typically used by smaller practices to reduce costs.
Third-party billing companies are considered Business Associates.
Requires a Business Associate Agreement before any PHI is shared.
In some cases, one covered entity (like a health clearinghouse) may act as a billing service for another—but still requires a BAA.
What Other Compliance Challenges Affect Medical Billing?
Medical Debt and Compliance
Millions of patients are billed directly, resulting in significant levels of medical debt:
In 2021, $220 billion in total debt.
Over 3 million people owed more than $10,000 each.
Local & State Regulations
The American Rescue Plan Act allocated funds to reduce medical debt burdens.
Some local laws cap medical bills based on income (e.g., Federal Poverty Level multipliers).
Healthcare providers must ensure compliance with both HIPAA and these localized billing rules.
What are the steps to achieve HIPAA compliance in billing based on best practices?
Conducting a risk assessment.
Developing HIPAA policies and procedures.
Training staff on privacy and security.
Implementing technical safeguards.
Using secure communication channels.
Signing Business Associate Agreements.
Enforcing the Minimum Necessary Rule.
Monitoring and auditing access logs.
Creating a breach notification protocol.
Keeping records and documentation up to date.
Final Thought: Why Is Compliance So Critical?
HIPAA compliance in medical billing is not just a legal obligation—it’s essential to safeguard patient trust, ensure operational integrity, and avoid costly penalties. As billing processes evolve and state laws introduce new complexities, vigilance and adaptability in compliance practices are more important than ever.
Why Choose Vital Health Services for HIPAA-Compliant Medical Billing?
At Vital Health Services, we understand that navigating the complexities of medical billing and HIPAA compliance can be overwhelming for healthcare providers. That’s why we offer specialized, secure, and scalable medical billing solutions designed to protect patient information, reduce administrative burden, and improve your revenue cycle.
With our deep industry expertise and commitment to compliance, we empower your practice to focus on what matters most—delivering exceptional patient care.
Key Benefits of Partnering with Vital Health Services
Full HIPAA Compliance
Every aspect of our billing process is aligned with HIPAA’s Privacy, Security, and Breach Notification Rules to ensure the highest level of data protection.
Improved Cash Flow
Our efficient claims management process helps you get paid faster with fewer denials and delays.
Dedicated Billing Experts
Work with certified billing professionals who understand payer rules, medical coding, and compliance intricacies.
Custom Solutions
Whether you’re a solo practitioner or a growing medical group, our services are tailored to meet your unique needs.
Real-Time Reporting
Gain full visibility into billing performance with transparent, actionable analytics.
Reduced Administrative Overhead
Let our team handle the paperwork so your staff can concentrate on patient care.